Where Do You Listen To Lung Sounds? You primarily listen to lung sounds on the anterior and posterior chest, as well as the lateral aspects, using a stethoscope; streetsounds.net offers a wealth of resources to help you discern normal from abnormal sounds. This guide delves into the nuances of chest auscultation, equipping you with the knowledge and skills to master this crucial diagnostic technique for respiratory assessment, enhance your acoustic perceptions, and explore advanced auscultatory techniques. Discover the vibrant sounds of the city with streetsounds.net, your ultimate destination for urban audio exploration and soundscapes.
Table of Contents
- What is Chest Auscultation and Why is it Important?
- Understanding Normal Lung Sounds: A Foundation for Auscultation
- Adventitious Lung Sounds: Identifying Abnormalities
- Anatomy and Physiology: How Lung Sounds are Produced and Transmitted
- Essential Equipment for Auscultation: Stethoscopes and Their Features
- Step-by-Step Guide to Performing Chest Auscultation
- Where on the Chest to Listen: Auscultation Points and Patterns
- Factors Affecting Lung Sounds: What to Consider During Auscultation
- Common Respiratory Conditions and Their Associated Lung Sounds
- Advanced Auscultation Techniques: Enhancing Your Diagnostic Skills
- Integrating Auscultation Findings with Other Diagnostic Tools
- The Role of Technology in Enhancing Auscultation Skills
- Challenges in Chest Auscultation and How to Overcome Them
- The Future of Auscultation: Innovations and Emerging Trends
- Street Sounds: Discovering Urban Soundscapes with streetsounds.net
- Frequently Asked Questions (FAQs) About Lung Sounds and Auscultation
1. What is Chest Auscultation and Why is it Important?
Chest auscultation is the process of listening to lung sounds with a stethoscope to assess the condition of the respiratory system. It’s a crucial diagnostic tool because it helps healthcare professionals identify a wide range of respiratory and cardiac conditions. According to a study by the American Thoracic Society, auscultation remains a fundamental skill for initial assessment, guiding further diagnostic testing and treatment decisions. With experience and a solid understanding of respiratory physiology, auscultation can provide valuable insights into a patient’s health status.
Why is it so important?
- Early detection: Auscultation can detect subtle changes in lung sounds that may indicate early stages of respiratory illness.
- Non-invasive: It’s a safe and painless procedure.
- Cost-effective: It requires only a stethoscope, making it accessible in various healthcare settings.
- Immediate feedback: Provides real-time information about the patient’s respiratory status.
- Guides treatment: Helps in determining the need for further investigations and appropriate interventions.
Auscultation is a cornerstone of physical examination, offering a direct and immediate window into the sounds of the lungs and airways.
2. Understanding Normal Lung Sounds: A Foundation for Auscultation
To accurately identify abnormal lung sounds, it’s essential to first understand what normal lung sounds should sound like. Normal breath sounds include vesicular, bronchovesicular, bronchial, and tracheal sounds. Each has distinct characteristics, intensity, pitch, and location where they are typically heard.
-
Vesicular Sounds: These are soft, breezy sounds heard over most of the lung fields. Inspiratory sounds are longer and louder than expiratory sounds.
 Vesicular Breath Sounds Lung Diagram
Vesicular Breath Sounds Lung Diagram -
Bronchovesicular Sounds: These are heard over the main bronchus area and around the upper right posterior chest. Inspiratory and expiratory sounds are equal in duration.
-
Bronchial Sounds: These are louder and higher-pitched, typically heard over the trachea. Expiratory sounds are longer than inspiratory sounds.
-
Tracheal Sounds: These are harsh, loud sounds heard over the trachea in the neck. Inspiratory and expiratory sounds are roughly equal.
Understanding the nuances of normal lung sounds provides a critical baseline for recognizing deviations that may indicate underlying pathology. By listening carefully and comparing sounds in different locations, clinicians can begin to differentiate between normal and abnormal respiratory function.
3. Adventitious Lung Sounds: Identifying Abnormalities
Adventitious lung sounds are abnormal sounds superimposed on normal breath sounds. These include crackles (rales), wheezes (rhonchi), stridor, and pleural rubs. Recognizing these sounds is vital for diagnosing various respiratory conditions.
-
Crackles (Rales): These are discontinuous, popping sounds heard during inspiration. They indicate fluid in the small airways or alveoli. Crackles are often associated with conditions like pneumonia, heart failure, and pulmonary fibrosis.
-
Wheezes (Rhonchi): These are continuous, high-pitched whistling sounds produced by narrowed airways. Wheezes are commonly heard in patients with asthma, COPD, and bronchitis.
-
Stridor: This is a high-pitched, harsh sound heard during inspiration, indicating upper airway obstruction. Stridor requires immediate attention, as it can signify a life-threatening condition such as epiglottitis or foreign body aspiration.
-
Pleural Rub: This is a grating, scratching sound caused by inflammation of the pleural lining. Pleural rubs are heard during both inspiration and expiration and are often associated with pleurisy.
Differentiating between these adventitious sounds requires practice and a keen ear. Each sound provides valuable clues about the underlying respiratory pathology.
4. Anatomy and Physiology: How Lung Sounds are Produced and Transmitted
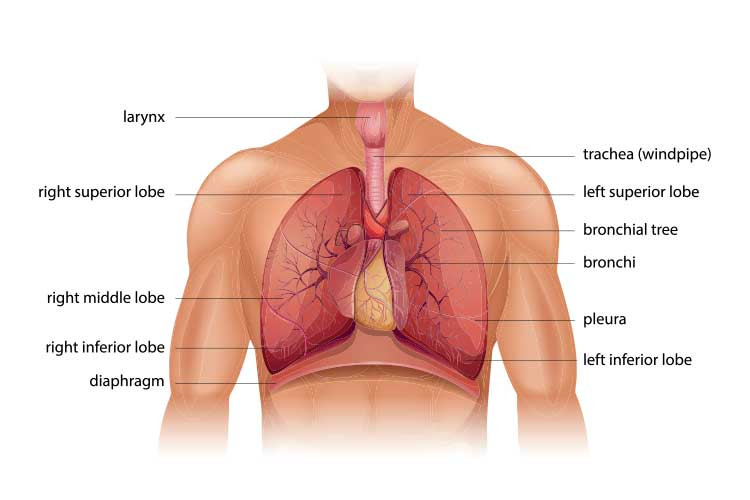
A thorough understanding of the anatomy and physiology of the respiratory system is crucial for interpreting lung sounds accurately. Air moves through the respiratory system, from the trachea to the bronchi and bronchioles, eventually reaching the alveoli, where gas exchange occurs. Lung sounds are produced by the movement of air through these structures.
The trachea and bronchi are larger airways that transmit sound more efficiently. The alveoli, being smaller and more numerous, produce softer, vesicular sounds. Changes in the airways, such as narrowing, obstruction, or inflammation, alter the way air moves and, consequently, the sounds produced. For example, narrowed airways cause wheezing due to turbulent airflow. Fluid in the alveoli produces crackles as air bubbles through the liquid.
Understanding the anatomical pathways and the physiological processes that generate lung sounds is essential for accurate auscultation and diagnosis. It allows healthcare professionals to correlate specific sounds with specific anatomical locations and physiological abnormalities.
5. Essential Equipment for Auscultation: Stethoscopes and Their Features
The stethoscope is the primary tool for chest auscultation. A quality stethoscope can make a significant difference in the ability to hear and differentiate subtle lung sounds. Key features to consider when choosing a stethoscope include:
- Acoustic Quality: The ability of the stethoscope to transmit sound accurately.
- Tubing Length and Material: Shorter, thicker tubing generally provides better sound transmission.
- Diaphragm and Bell: The diaphragm is used for high-frequency sounds, while the bell is used for low-frequency sounds.
- Earpieces: Should fit comfortably and provide a good seal to block out external noise.
Some popular stethoscope brands include Littmann, Welch Allyn, and MDF Instruments. Littmann stethoscopes are widely regarded for their acoustic performance and durability. Welch Allyn offers stethoscopes with innovative features such as ambient noise reduction. MDF Instruments provides high-quality stethoscopes at a more affordable price point.
Choosing the right stethoscope is a personal decision based on individual preferences and needs. However, investing in a quality instrument can greatly enhance the accuracy and effectiveness of chest auscultation.
6. Step-by-Step Guide to Performing Chest Auscultation
Performing chest auscultation requires a systematic approach to ensure thorough and accurate assessment. Here is a step-by-step guide:
- Preparation:
- Introduce yourself to the patient and explain the procedure.
- Ensure the patient is comfortable and in a sitting position if possible.
- Provide privacy and drape the patient appropriately.
- Warm the stethoscope diaphragm to avoid startling the patient.
- Technique:
- Instruct the patient to breathe slowly and deeply through their mouth.
- Place the stethoscope diaphragm firmly against the patient’s bare chest.
- Listen to at least one full breath cycle (inspiration and expiration) at each location.
- Compare sounds from side to side at each location.
- Systematically move across the chest, following a predetermined pattern.
- Locations:
- Listen to the anterior, posterior, and lateral chest.
- Avoid listening over bone (e.g., scapula) or clothing.
- Pay attention to the intensity, pitch, duration, and quality of the sounds.
- Identify any adventitious sounds.
- Documentation:
- Record your findings in the patient’s chart, including the location and characteristics of any abnormal sounds.
- Note any factors that may affect lung sounds, such as body position or underlying medical conditions.
Following these steps ensures a comprehensive and consistent approach to chest auscultation, improving the accuracy and reliability of the assessment.
7. Where on the Chest to Listen: Auscultation Points and Patterns
To ensure a thorough assessment, it’s important to listen to specific locations on the chest in a systematic pattern. Auscultation points are typically located on the anterior, posterior, and lateral chest walls.
-
Anterior Chest: Begin above the clavicles, moving down and comparing side to side at each level. Listen at least four points on each side.
-
Posterior Chest: Start at the apices of the lungs, moving down and comparing side to side. Listen at least six points on each side, avoiding the scapula.
-
Lateral Chest: Listen in the mid-axillary line, comparing side to side.
A common auscultation pattern is the “ladder” pattern, where you move systematically down the chest, comparing each side at each level. It’s important to listen at each location for at least one full breath cycle to assess the inspiratory and expiratory sounds. The number of locations may vary based on patient conditions and individual assessment needs.
8. Factors Affecting Lung Sounds: What to Consider During Auscultation
Several factors can influence lung sounds and affect the accuracy of auscultation. These include:
- Body Position: Sitting upright is generally the best position for auscultation, as it allows for optimal lung expansion.
- Patient Cooperation: If the patient is unable to follow instructions or breathe deeply, it can be difficult to assess lung sounds accurately.
- Environmental Noise: A quiet environment is essential for hearing subtle lung sounds.
- Chest Wall Thickness: Obesity or increased muscle mass can dampen lung sounds.
- Underlying Medical Conditions: Conditions such as scoliosis or chest wall deformities can alter lung sounds.
It’s important to be aware of these factors and take them into consideration when interpreting lung sounds. Adjusting the technique, such as having the patient lean forward or using the bell of the stethoscope for low-frequency sounds, can help overcome some of these challenges.
9. Common Respiratory Conditions and Their Associated Lung Sounds
Different respiratory conditions produce distinct lung sounds that can aid in diagnosis. Some common conditions and their associated sounds include:
| Condition | Lung Sounds |
|---|---|
| Pneumonia | Crackles (rales) in the affected area, bronchial breath sounds, increased tactile fremitus |
| Asthma | Wheezes (rhonchi), prolonged expiration, decreased breath sounds |
| COPD | Wheezes (rhonchi), decreased breath sounds, prolonged expiration |
| Heart Failure | Crackles (rales) in the bases of the lungs, possible wheezes |
| Pulmonary Fibrosis | Dry, crackling sounds (Velcro rales) |
| Pleural Effusion | Decreased or absent breath sounds, possible pleural rub |
| Pneumothorax | Absent breath sounds on the affected side, hyperresonance to percussion |
| Bronchitis | Rhonchi that may clear with coughing |
Recognizing these patterns can help narrow the differential diagnosis and guide further investigations.
10. Advanced Auscultation Techniques: Enhancing Your Diagnostic Skills
To further refine auscultation skills, consider incorporating these advanced techniques:
- Forced Expiratory Technique: Listen during a forced expiration to accentuate wheezes.
- Egophony: Have the patient say “EE” while listening over the lungs. If it sounds like “AA,” it indicates consolidation.
- Whispered Pectoriloquy: Have the patient whisper a phrase while listening over the lungs. If it’s heard clearly, it suggests consolidation.
- Bronchophony: Have the patient say “99” while listening over the lungs. Increased clarity suggests consolidation.
- Comparative Auscultation: Compare lung sounds from side to side and top to bottom to identify subtle differences.
These techniques can help detect subtle abnormalities and improve diagnostic accuracy.
11. Integrating Auscultation Findings with Other Diagnostic Tools
Auscultation is most effective when integrated with other diagnostic tools and clinical information. It should be part of a comprehensive assessment that includes:
- Patient History: Information about symptoms, medical history, and risk factors.
- Physical Examination: Inspection, palpation, and percussion of the chest.
- Imaging Studies: Chest X-rays, CT scans, and MRIs.
- Pulmonary Function Tests: Spirometry and lung volume measurements.
- Arterial Blood Gases: Assessment of oxygenation and ventilation.
By combining auscultation findings with other data, healthcare professionals can develop a more complete and accurate picture of the patient’s respiratory status.
12. The Role of Technology in Enhancing Auscultation Skills
Technology is playing an increasingly important role in enhancing auscultation skills and improving diagnostic accuracy. Electronic stethoscopes can amplify sounds, filter out background noise, and record lung sounds for later review. Some electronic stethoscopes also offer features such as:
- Sound Visualization: Displaying lung sounds as waveforms or spectrograms.
- Automated Analysis: Using algorithms to identify abnormal sounds.
- Telemedicine Capabilities: Transmitting lung sounds remotely for consultation with specialists.
Furthermore, online resources and simulation tools can help healthcare professionals practice and improve their auscultation skills.
13. Challenges in Chest Auscultation and How to Overcome Them
Despite its value, chest auscultation presents several challenges:
- Subjectivity: Interpretation of lung sounds can vary among different observers.
- Hearing Impairment: Healthcare professionals with hearing loss may have difficulty auscultating.
- Environmental Noise: Noisy environments can interfere with auscultation.
- Patient Factors: Obesity, chest wall deformities, and patient cooperation can affect the accuracy of auscultation.
To overcome these challenges:
- Practice Regularly: Consistent practice is essential for developing auscultation skills.
- Seek Feedback: Ask experienced colleagues for feedback on your technique and interpretations.
- Use Technology: Consider using electronic stethoscopes to amplify sounds and filter out noise.
- Create a Quiet Environment: Minimize distractions and background noise during auscultation.
- Adapt Technique: Adjust your technique based on patient factors and environmental conditions.
By addressing these challenges and continuously striving to improve, healthcare professionals can maximize the effectiveness of chest auscultation.
14. The Future of Auscultation: Innovations and Emerging Trends
The future of auscultation is likely to be shaped by several innovations and emerging trends:
- Artificial Intelligence (AI): AI algorithms are being developed to analyze lung sounds and assist in diagnosis.
- Wearable Sensors: Wearable devices that continuously monitor lung sounds may become available.
- Tele-Auscultation: Remote auscultation using electronic stethoscopes and telemedicine platforms is expanding.
- Personalized Medicine: Auscultation may be used to tailor treatment plans based on individual lung sound profiles.
These advancements promise to enhance the accuracy, accessibility, and effectiveness of auscultation, further solidifying its role in respiratory assessment.
15. Street Sounds: Discovering Urban Soundscapes with streetsounds.net
While mastering the subtleties of lung sounds is critical for healthcare professionals, the world of sound extends far beyond the clinical setting. At streetsounds.net, we invite you to explore the rich and diverse soundscapes of urban environments. From the rhythmic pulse of city traffic to the melodic busking in subway stations, street sounds offer a unique lens through which to experience and understand the world around us.
Whether you’re a sound designer seeking inspiration, a filmmaker aiming for authenticity, or simply a curious listener, streetsounds.net provides a curated collection of high-quality recordings that capture the essence of urban life. Our library features:
- Ambiences: Immersive recordings of bustling city streets, quiet residential neighborhoods, and vibrant public spaces.
- Specific Sounds: Targeted recordings of individual sound events, such as car horns, construction noise, and street performers.
- Themed Collections: Curated sets of sounds that evoke specific urban experiences, such as a rainy night in New York or a sunny afternoon in San Francisco.
Explore our collection and let the sounds of the city inspire your creativity.
Discover urban audio exploration at Address: 726 Broadway, New York, NY 10003, United States. Phone: +1 (212) 998-8550. Website: streetsounds.net.
16. Frequently Asked Questions (FAQs) About Lung Sounds and Auscultation
- What are the four normal breath sounds? Vesicular, bronchovesicular, bronchial, and tracheal sounds.
- How do crackles sound? Discontinuous, popping sounds, like rubbing strands of hair together near your ear.
- What causes wheezing? Narrowed airways, often due to asthma or COPD.
- Where is the best place to listen for vesicular breath sounds? Over the peripheral lung fields.
- What does stridor indicate? Upper airway obstruction, a medical emergency.
- Can obesity affect lung sounds? Yes, excess tissue can dampen lung sounds.
- What is egophony? When “EE” sounds like “AA” during auscultation, indicating lung consolidation.
- Why is it important to warm the stethoscope before auscultation? To avoid startling the patient and causing muscle tension that could affect lung sounds.
- How does pneumonia affect lung sounds? It often causes crackles in the affected area.
- Is auscultation alone sufficient for diagnosing respiratory conditions? No, it should be combined with other diagnostic tools and clinical information.
By understanding these key concepts and frequently asked questions, you can enhance your knowledge and skills in chest auscultation and better serve your patients. Now that you know where to listen to lung sounds, it’s time to refine your skills and explore the fascinating world of respiratory assessment. Visit streetsounds.net today and discover the sounds that shape our world.